Welcome to the Department of Immunology & Microbiology
MISSION STATEMENT
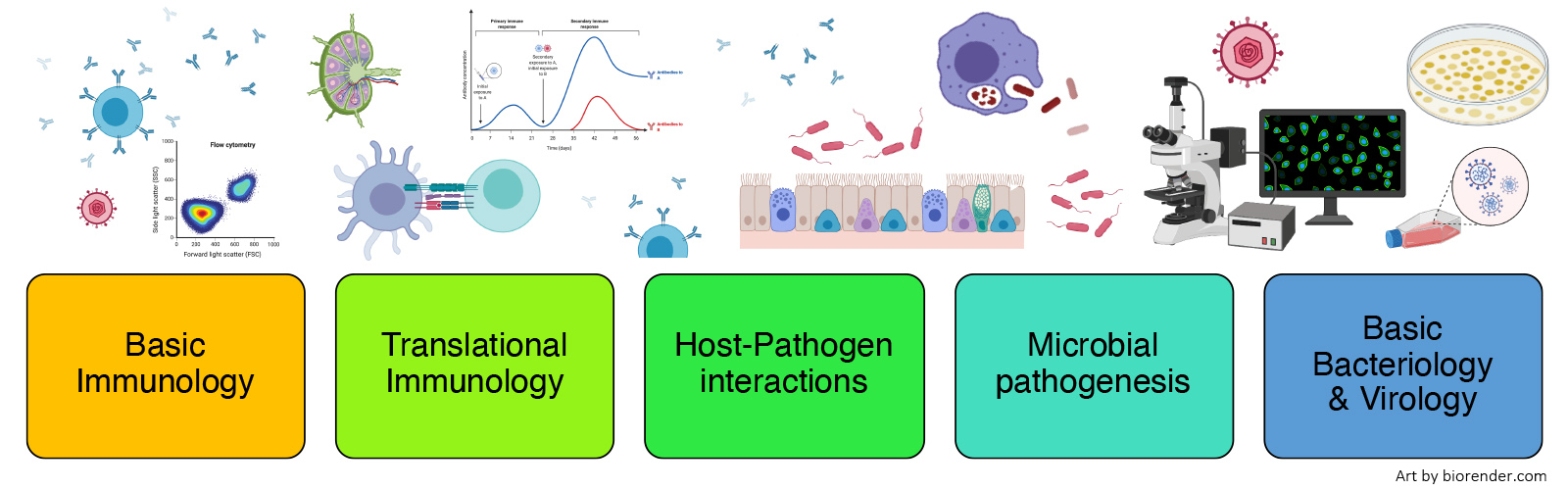
To stimulate leading-edge research and scientific training in a diverse and welcoming community. We focus our collective expertise on fundamental mechanisms in immunity and infection, and work together to transform the power of scientific discovery into novel therapies for infectious diseases, autoimmunity and cancer.




05/23/2025 | Meet the Scientist: Thomas ‘Tem’ Morrison focuses on how dangerous viruses infect humans and how our bodies work to clear them in “Lifeguard on Duty: Better Understanding the Body’s First Responders”

04/23/25 | READ CU Anschutz Today featuring Assistant Research Professor, Jared Klarquist, PhD in "B Cells Found to Be Crucial for Long-Term Vaccine Protection, New Study Shows" here discussing new insight from a recently published study in The Journal of Clinical Investigation.

3/19/25 | This month's Research Achievement Highlights (REACH) forum featured various presenters, including Aimee Pugh Bernard, PhD. They shared tips on how to navigate medical misinformation through connection. You can read a summary of the forum in the article linked below.

STEM Poster Day 2025 presenters, volunteers and Project Bridge Colorado organizers pose on the steps of the Colorado State Capitol in Denver on March 11, 2025. Photo courtesy of Rachael Kostelecky.
3/13/2025 | STEM Poster Day Brings Science Under the Gold Dome of the Colorado Capitol
Young researchers from the CU School of Medicine and others showcased their work at the event.

3/12/2025 | Researchers from the University of Colorado Anschutz Medical Campus and funded by the NIH, studied a new method to deliver antibiotics, specifically gentamicin, directly into the bladder tissue to better treat UTIs.

03/03/2025 | Cu Anschutz Basic Science Departments Chairs, Leslie Berg, PhD, Julie Cooper, PhD, David DiGregorio, PhD, Heide Ford PhD, Casey Greene, PhD Wendy Macklin, PhD, and Science Communicator, Aimee Pugh Bernard, PhD wrote an Op-Ed about NIH funding needs titled, "Opinion: The Critical Need for Science Funding" which was featured in the online newspaper Front Porch.
READ IT HERE

From A Message from Dean Sampson | July 21, 2025
"Curtis J. Henry, PhD, Associate Professor of Immunology and Microbiology, and James DeGregori, PhD, Professor of Biochemistry and Molecular Genetics, are corresponding authors of a review article, “Modelling the ageing dependence of cancer evolutionary trajectories,” published July 10 by Nature Reviews Cancer. Dr. Henry is Deputy Associate Director, and Dr. DeGregori is Deputy Director of the CU Cancer Center."

4/17/2025 | Various authors including Cameron Manes, Ross M. Kedl, Jared Klarquist and other researchers from the CU Anschutz School of Medicine published their study, “B cells shape naïve CD8 T cell programming,” in The Journal of Clinical Investigation.

3/24/2025 | Jenna J. Guthmiller, PhD, Assistant Professor of Immunology and Microbiology, is a corresponding author of an article, “Long-lasting B cell convergence to distinct broadly reactive epitopes following vaccination with chimeric influenza virus hemagglutinins,” published March 24 by Immunity.

3/7/2025 | Kyla Ost, PhD, Assistant Professor of Immunology and Microbiology, is a co-author of a research article, “Neonatal fungi promote lifelong metabolic health through macrophage-dependent β cell development,” published by Science.

2025 Student Leader of the Year
Student Graduate
Rachael Kostelecky
This award recognizes a student leader who has provided exemplary service, commitment, and strong leadership to a student organization.

2025 President's Inclusive Excellence Award
Student Graduate
Gabrielle Vragel
"Gabrie's respectful consideration of both peers and leadership and her undaunted spirit make her a very impactful student leader and change-maker."

2025 WINNER: The Joseph Addison Sewall Award
Leslie J. Berg, PhD
Professor and Chair | Immunology and Microbiology Department

Dr. Emma Sheriff, former PhD student in the Duerkop lab, had her paper entitled “Enterococcal quorum-controlled protease alters phage infection” selected as the best paper of 2024 published in FEMS Microbes.
Get to Know Curtis Henry, PhD, CU Cancer Center deputy associate director, Office of EAS
Curtis Henry, PhD, developed a passion for science early, inspired by his family and his cousin’s battle with leukemia. Now, he studies how comorbidities impact the immune system’s fight against cancer. Through patience and perseverance, he’s turned challenges into opportunities, driving his mission to find better treatments.
Watch the Interview on LinkedIn
AAI Lifetime Achievement Award

Leslie Berg, PhD is the recipient of the 2025 Lifetime Achievement Award, granted, “In recognition of a remarkable career of scientific achievement and contributions to AAI and the field of immunology.”
AAI ASPIRE Award

Jenna Guthmiller, PhD is a recipient of the 2025 AAI ASPIRE Award, granted “For early-career research accomplishments and professional promise in the field of immunology.”
2025 CU Anschutz Research Award

Raul Torres, Ph.D. has been selected to receive the Research Mentor Award for the 2025 CU Anschutz Research Award program and the award ceremony will be February 19th at 4 pm in the Elliman Conference Center.
We are a CU Anschutz Medical Campus Basic Science Departments!
To learn about the discoveries that are shaping the future of medicine...

Immunology Microbiology (SOM)
CU Anschutz
Research I North
12800 East 19th Avenue
Mail Stop 8333
Aurora, CO 80045
303-724-4224