Referring Physician Information
University of Colorado Department of Ophthalmology
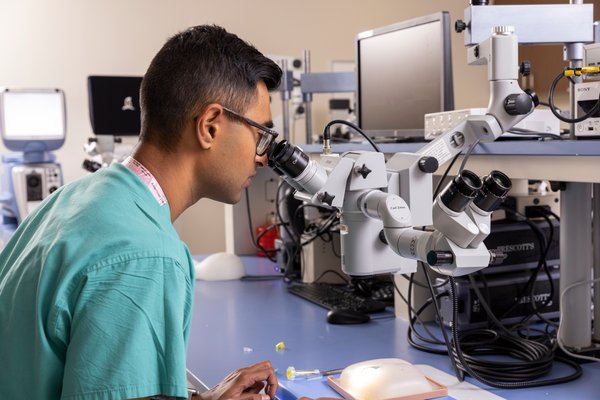
The technological innovations conceived and developed by Departmental faculty have changed the practice of eye care throughout the world. Our educational programs train the next generation of leaders in ophthalmology. We have invested heavily in tracking our clinical outcomes, and we are proud that our clinicians perform at the highest levels in their respective fields.
- Read the full letter from our chair, Naresh Mandava, MD, here.
Make an Appointment
By the Numbers
163
Faculty Research, and Administration Staff
166,800+
Unique Patient Visits by Our Faculty in FY2023
31
Residents and Fellows
$16M+
Sponsored Projects from FY2021-2023
Newsroom
Loading items....
See Us In The News
Loading items....