Division of Infectious Diseases
A multidisciplinary team of clinicians, educators, and scientists working to improve the prevention and treatment of infectious diseases
Welcome
Our faculty, more than 80 and growing, are dedicated to clinical care, education, and research. We strive to promote the specialty of infectious diseases (ID) through impactful clinical care that improves lives; adding value through antibiotic stewardship, diagnostic stewardship, and infection prevention; educating the next generation of clinicians and ID physicians; and discovery and dissemination of world class research.

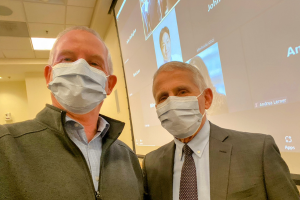
Edward Stenehjem, MD, MSc
Interim Division Head, Infectious Diseases
Executive Vice Chair, Department of Medicine