Ranked #8 for Top Medical Schools
U.S. News and World Report ranks us #8 for top primary care medical schools.
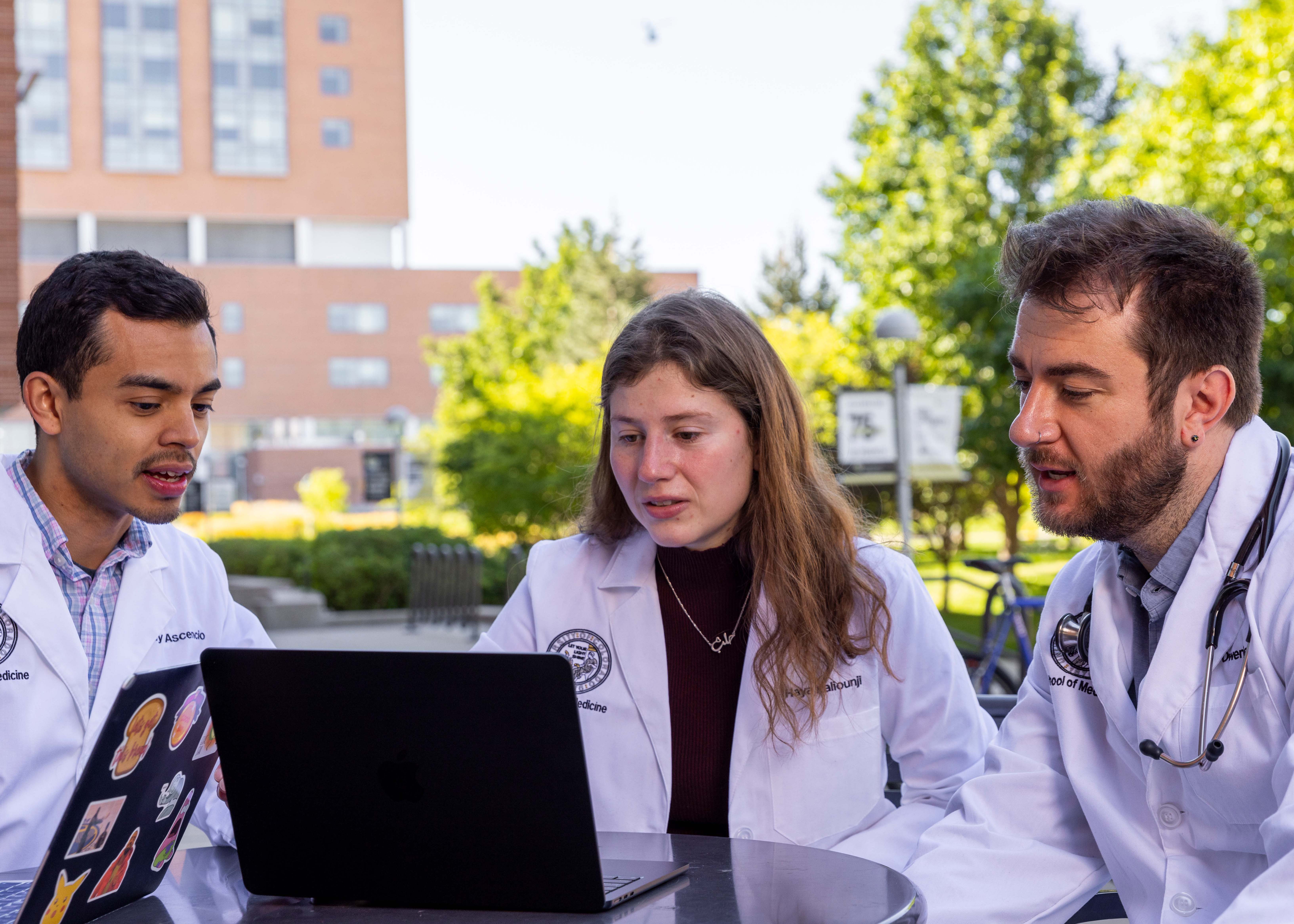
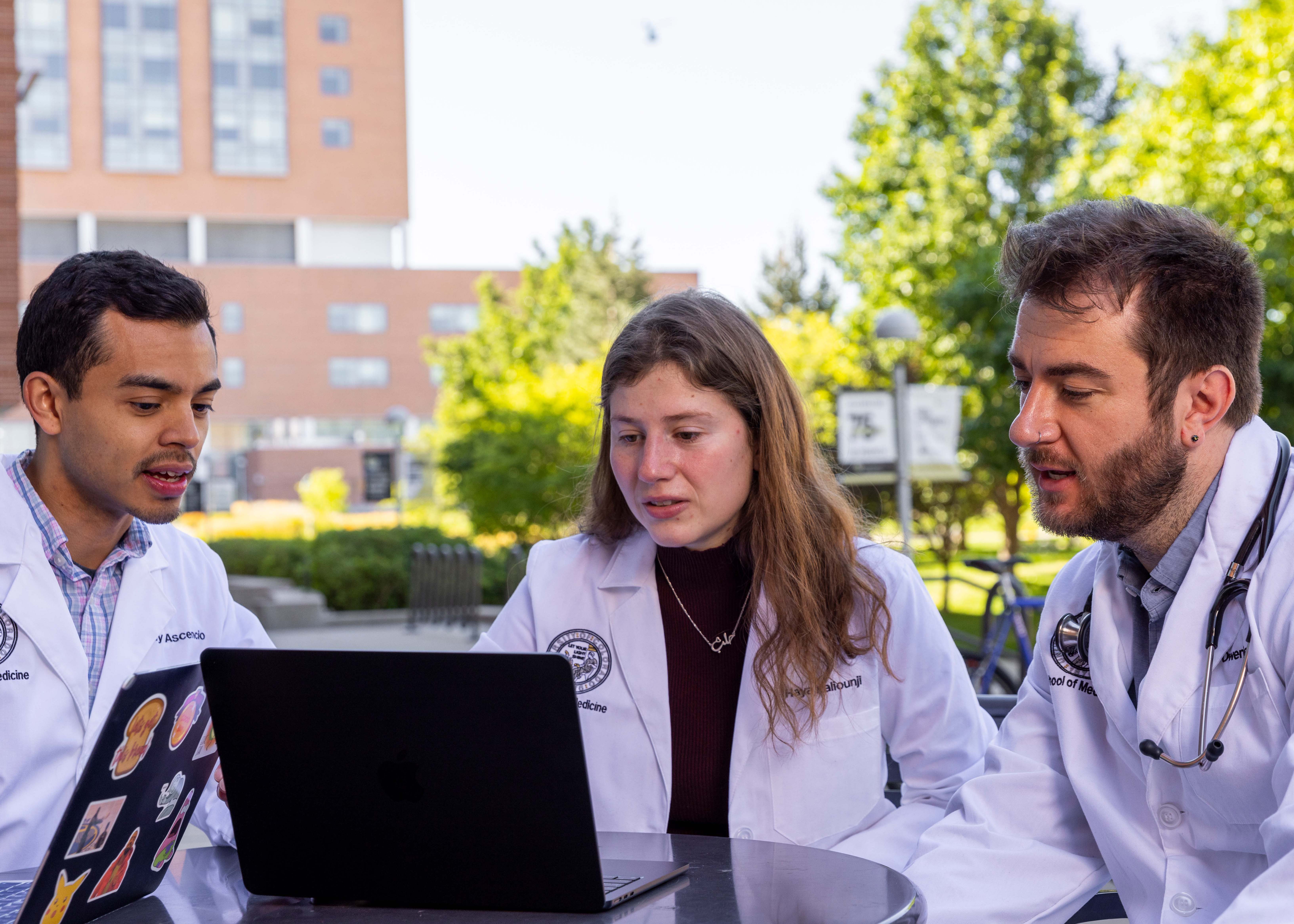
It is a great privilege for me to serve as the 6th Chair of the Department of Medicine at the University of Colorado Anschutz Medical Campus, the largest clinical department in the School of Medicine. Since its establishment in 1883, our Department has
been an innovative leader in the advancement of patient care, education and research.
With more than 1,000 faculty, 192 residents and 200 fellows distributed in 14 divisions, our clinical, research and academic programs attract the
best providers, investigators, staff and students from around the world who are transforming the future of health care.
As Chair, I remain committed to evolving the Department and meeting the ever-changing needs of healthcare and our
patients. I invite you to explore our website to learn more about our many programs, offerings, centers of excellence and innovations.
Vineet Chopra, MD, MSc
Robert W. Schrier Chair of Medicine
Ranked #8 for Top Medical Schools
U.S. News and World Report ranks us #8 for top primary care medical schools.
Cared for 49% of UCHealth Admissions
255,235 outpatient visits were conducted by our faculty, fellows, and residents.

Awarded $114 Million in Research Funding
Our faculty has been a part of 2,555 peer-reviewed research publications.
Our future is brighter and better than it has ever been. Scroll through the pages of our latest annual report to see how we're advancing clinical excellence, performing cutting-edge research, and teaching the next generation of physicians.