Colorado's Most Trusted Orthopedic Care for Adults and Children
The University of Colorado Orthopedics team delivering patient care is also tirelessly creating new discoveries in orthopedic research and training the next generation of orthopedic leaders in the most advanced surgical and non-invasive techniques and treatment options.
All within a network of healthcare partners ranked among the best in the Rocky Mountain region and globally.
#1
#1
Adult Hospital in Colorado
UCHealth University of Colorado Hospital
Pediatric Hospital in Colorado & Rocky Mtn Region
Children's Hospital Colorado
*Rankings from the 2022-23, 2023-24 U.S. News & World Report's 'Best Hospitals.'

200,000+
annual outpatient visits
19,000+
annual surgical cases
184
physicians & researchers
18
Front Range Locations

Our doctors specialize in compassionate, comprehensive care centered around you
Your expert team of orthopedic physicians, physical therapists, and advanced practice providers will tailor a plan for your specific needs and goals.
From routine care to the most complex cases, we treat more adults and children with orthopedic conditions than any provider in our region.
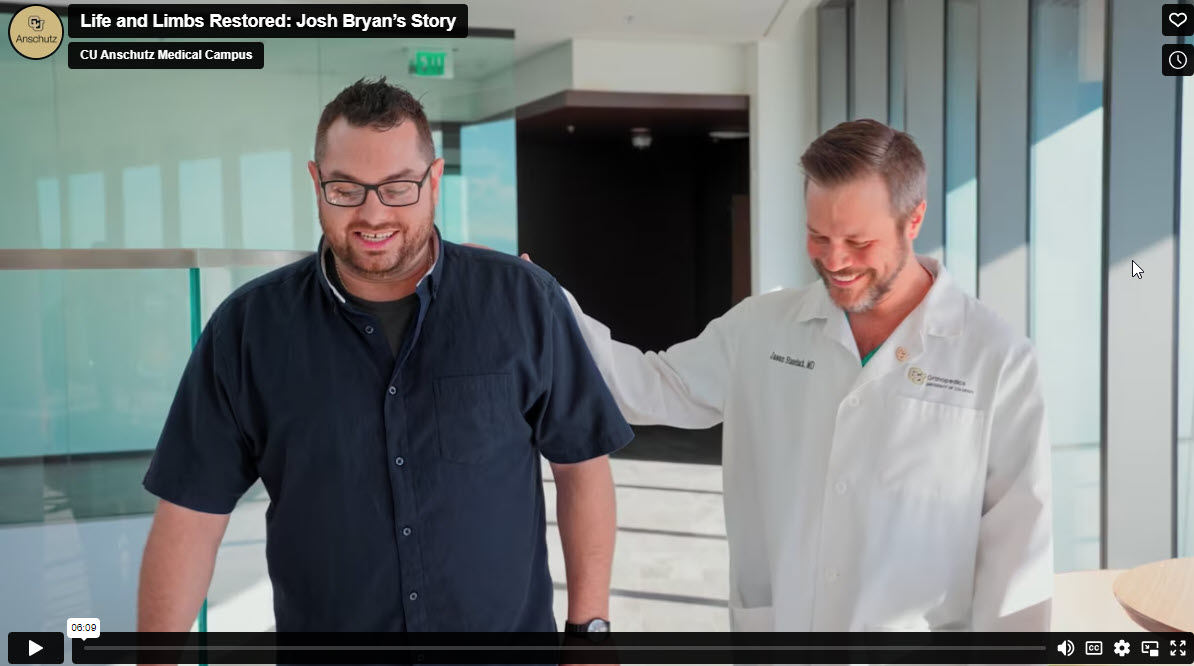
Mission in Motion
Keeping you moving is our mission.
Learn about the latest from your team of trusted experts in orthopedics.