Welcome to the Department of Immunology & Microbiology
To stimulate leading-edge research and scientific training in a diverse and welcoming community. We focus our collective expertise on fundamental mechanisms in immunity and infection, and work together to transform the power of scientific discovery into novel therapies for infectious diseases, autoimmunity and cancer.

Leslie Berg, PhD
Professor, Chair
T cell activation, differentiation, and responses to infection and how these processes are regulated by T cell antigen receptor signaling
Linda van Dyk, PhD
Professor, Vice Chair
Genetic and molecular approaches to infection and pathogenesis by lymphotropic herpesviruses-
Research In Progress 2024: Megan Stumpf & Alyx Job
| 10:30 AM - 11:30 AMRoom Number: Heither Hall at NJH or Hensel Phelps at AMC
Research I North
12800 East 19th Avenue
Aurora, CO
-
Science Communication Workshop
| 04:00 PM - 05:30 PM
-
Friday Seminar Series: Jamie Rossjohn, FFA FAHMS FLSW FMedSci FRS
| 10:00 AM - 11:00 AMRoom Number: Hensel Phelps East Auditorium, P18 - 1000
Research I North
12800 East 19th Avenue
Aurora, CO
-
Friday Seminar Series: David Masopust
| 12:00 PM - 01:00 PMRoom Number: Hensel Phelps East Auditorium, P18 - 1000
Research I North
12800 East 19th Avenue
Aurora, CO
-
Research In Progress 2024
| 10:30 AM - 11:30 AM
Department News
The Office of Research Education is continuing its partnership with the Tattered Cover Book Store to provide talks on the basic science featured in current books. The next event, at 6 p.m Thursday, January 26, will feature Aimee Bernard, PhD, assistant professor of immunology and microbiology, and Gabriella Albert and Marina Good, two PhD students in the Office of Research Education’s Immunology Program. Aimee, Gabi, and Marina will lead a session, “Your Shot at Protection: How Vaccines Train the Immune System to Fight Disease.” They will present a primer on the science and take questions from the audience. This outreach program features our exceptional students and faculty and makes stronger connections with the community we serve. Many thanks to the Tattered Cover for hosting the event at their store at 2526 E. Colfax Ave., Denver. Also, thanks to the Office of Research Education for creating this collaboration with one of Denver’s leading cultural institutions.
Congratulations to Aimee Bernard, PhD for winning the 2024 Chancellor’s Teaching Recognition Award for the School of Medicine!

Research from Andrés Vazquez-Torres’s Lab was published in Science journal, Vol 384, Issue 6691. Read Prophage terminase with tRNase activity sensitizes Salmonella enterica to oxidative stress by clicking the button below.
READ HERE
Kelly Doran received a fundable score on an R21 for a new project looking at the impact of a gut commensal bacterium on Group B streptococcus colonization and disease.
Kelly Doran received a contract from Intralytix to study phage therapy in the vaginal tract
Madeline Akbari – a graduate student in the Microbiology program in the Doran lab received a fundable score on her F31
Ross Kedl’s article, Evidence for Aerosol Transfer of SARS-CoV-2–Specific Humoral Immunity” was the most-read ImmunoHorizons (Volume 7, Issue 5) article in 2023.
READ HERE
Breck A. Duerkop, PhD, associate professor of immunology and microbiology, is corresponding author of an article published April 1 by Cell Host & Microbe that provides a resource to better understand the genomes of the microbiota. Breck and his co-authors establish a framework for studying insertion sequence elements within the microbiota. Insertion sequence elements are mobile genetic elements in bacterial genomes that support adaptation. The article offers a first step toward understanding how these elements contribute to the function of the microbiota impacting human health. PhD student Joshua M. Kirsch is a co-author of the study.
Aimee Bernard, PhD (in collaboration with Eduardo Davila and Merdith Tennis) received a fundable score for their R25 NCI Youth Enjoy Science (YES) grant application!
Chuangqi Wang, PhD received a Pilot Grant award from the Center for Mucosal Immunology and Rheumatic Disease Pathogenesis (CMIR), School of Medicine. This pilot grant will focus on investigating the EBV effects on RA progression by deeply profiling the humoral immune response of EBV and RA autoantibodies using a systems serology platform.
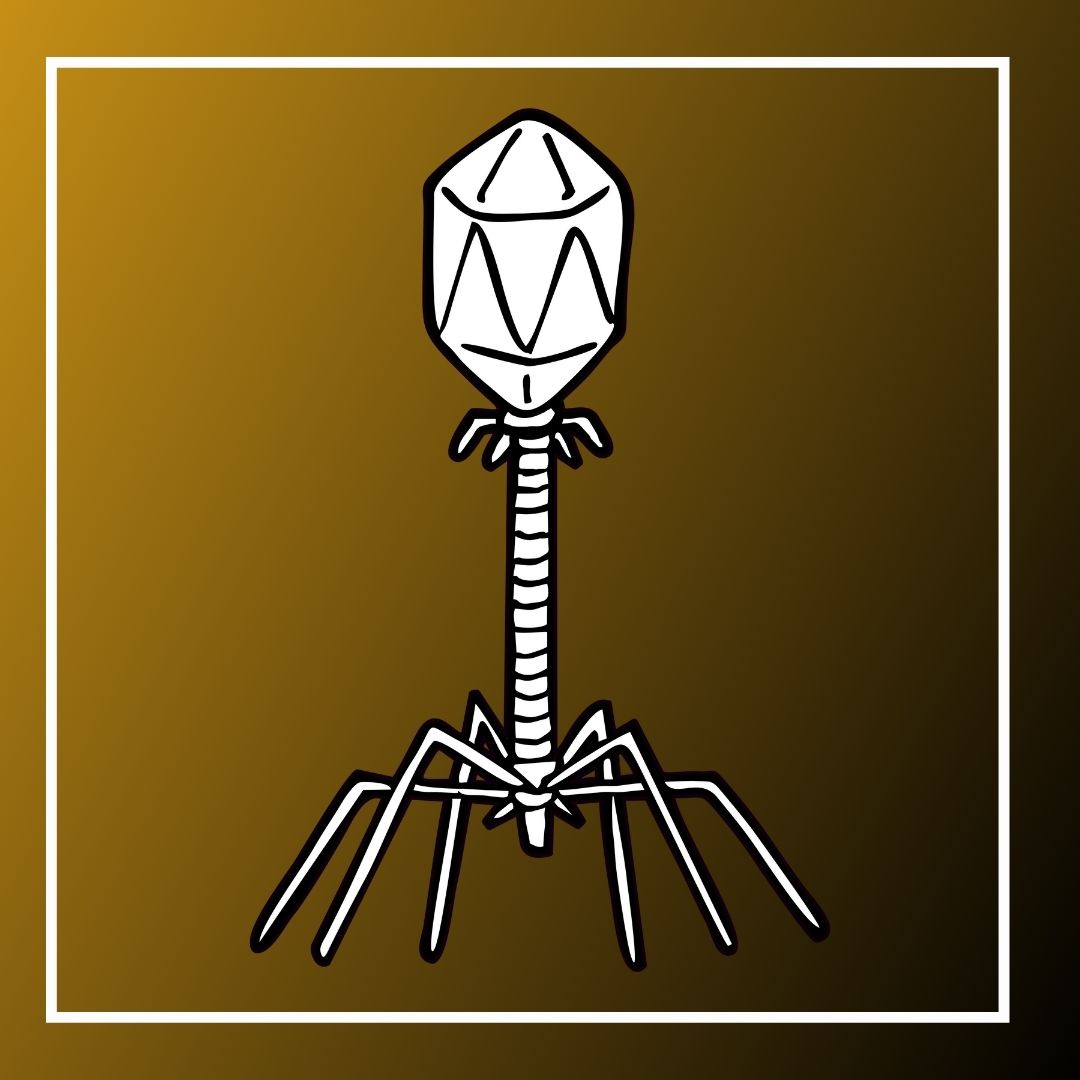
A paper by Breck Duerkop, PhD's group and colleagues at the University of Pittsburgh was covered in a recent article in Wired magazine.
Jeremy Fleck, Immunology PhD student spoke with faculty member, Dr. Raul Torres, on episode 74 of his podcast, Flying Intuition. Learn about Raul's path into science and support Jeremy by giving it a listen!

Aimee Bernard, PhD was interviewed alongside Akiko Iwasaki on 'The Immunology Podcast' about 'Public Outreach'
Article by Leslie J. Berg, PhD featured in Open Access Government January 2024: Understanding T lymphocytes inner workings to harness therapeutic potential